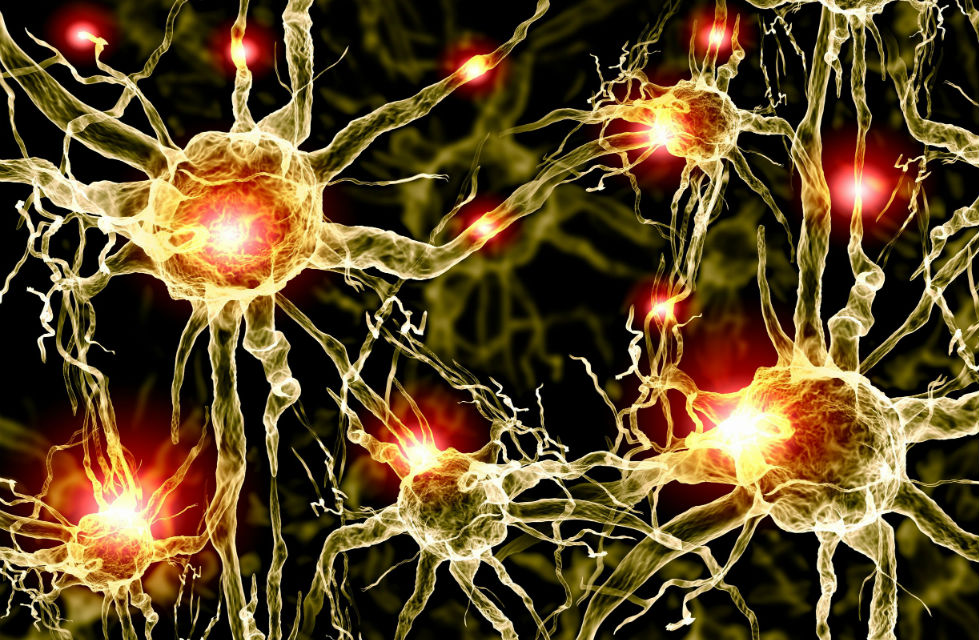
Brains “on Fire”
Written by Dr Ben Marlow, the Consultant Paediatrician at Brainstorm Health®, for the Autism Eye Magazine.
Ground-breaking research is giving weight to the view that when the immune system goes wrong children can tip into autism. Dr Ben Marlow, paediatrician and father to Freddie, who has a diagnosis of autism, describes the effect the process has on the developing brain.
Autism is an umbrella term
Autism is an umbrella term with many subtypes. The heterogeneous nature of the phenotype (in other words, the way that it manifests in an individual) is further complicated by the unpredictable way that it affects the body and the nervous system.
There are frequent associations with certain syndromes and many ‘risk genes’ have been identified. Nevertheless, there is emerging evidence that a dysregulated immune system can have devastating effects on the developing brain.1
Medicine is entering a new age of neuropsychiatry, which is the branch of medicine dealing with diseases involving the mind and nervous system. It is challenging traditionally held beliefs about the underlying causes of behaviour. In turn, this is leading to a range of new therapies that have not previously been explored.
Microglia start to cause trouble – attacking neurons and synapses within the brain that shouldn’t be broken down. This creates a toxic soup
My particular interest is looking at the association between the immune system and the nervous system, and in particular at a cohort of children with autism where the immune system has become dysregulated and hyperactive.
The children with this ‘immune subtype’ of autism tend to be more on the severe end of the spectrum. They have difficulties with language and stereotypical behaviour. They also have sequelae of systemic disease, in other words, abnormal conditions resulting from a previous disease. This can be mitochondrial dysfunction (which affects the body’s use of energy), bowel problems and marked hypersensitivities.
A ‘hyperactive’ immune system
Epidemiological studies (the branch of medicine dealing with the incidence and prevalence of disease in large populations) have shown there is an association between certain inflammatory disease in the mother or child and the risk of autism, especially with regression.2
The maternal immune system can be activated via infection or other pathways and trigger an inflammatory response. This can lead to an increase in inflammatory molecules such as Interleukin 1B, IL-6, IL-17 and TNF.1
It can also increase the number of other cells. Among these are mast cells, which are present in connective tissue and release heparin, histamine, serotonin and other molecules during inflammation and allergic reactions. These cell-derived messengers, called inflammatory mediators, act on blood vessels, inflammatory cells or other cells to contribute to an inflammatory response.
Mast cells can also increase the permeability of the blood-brain barrier. This can cause inflammatory mediators to enter the brain.
‘Brain fire’
Once these inflammatory mediators are in the brain, there are immune surveillance molecules called microglia that start to increase in number. Normally, microglia police the body’s cerebrospinal fluid within the brain looking for signs of infection – they are part of the innate immune system. If they find anything that shouldn’t be there they can manufacture chemicals to kill the offending bacteria or invader. The M1 subtype can be particularly destructive.
In this inflammatory subtype of ASD, it is thought that these microglia start to cause trouble – attacking neurons and synapses within the brain that shouldn’t be broken down. This creates a toxic soup of inflammatory mediators and abnormal neuronal firing. Professor Theoharides (Tufts, in Boston) refers to this as ‘brain fire’. It results in disorganised, ineffective neural connectivity and neuronal loss.
The systemic fallout
As a consequence of the microglial overactivity, the production of nitric oxide increases. This can have an impact on a variety of organ systems.
Systemic features in this cohort of children include headache, higher rates of infection due to the reduction and impairment of specific cells within the immune system called ‘Natural Killer’ (NK) cells, seizures and abnormal brain waves called Subepileptiform Discharges, or SEDs.3 Other features can be an increased incidence of food allergies and gut problems.
Features in this cohort of children include headache, higher rates of infection… seizures and abnormal brain waves… food allergies and gut problems
Nitric oxide in high levels has also been shown to impact the function of mitochondria, which are organelles responsible for the generation of energy within the body.
Future directions – putting the fire out
The time has come for the scientific community and clinicians to acknowledge that there are a large proportion of children and their families with a diagnosis of ASD whose symptoms and other co-existing conditions could be greatly improved by addressing the issue of immune dysfunction.
Dampening down this inflammatory cascade should be seen as a target in this cohort of children. Other specific targets could be modulating microglial function, correcting the excitatory/inhibitory imbalance within the nervous system, or treating subepileptiform discharges (SEDs).
The presence of SEDs is widespread and may be a precursor to seizures. Studies now show treating SEDs before they progress to seizures may mark a significant change in traditional views held about epilepsy.3
Many other neuropsychiatric diseases such as schizophrenia, multiple sclerosis and Parkinson’s have more funding and research motivation. This research involves similar fields of chronic neuroinflammation and microglial activation. Autism deserves to have the same spotlight and scientific interest, translating scientific work into action.
References
- Theoharides et al: ‘Atopic diseases and inflammation of the brain in the pathogenesis of autistic spectrum disorders’, Translational Psychiatry, 2016
- Scott et al, 2017: ‘Clinical cues for autoimmunity and neuroinflammation in patients with autistic regression’, DMCN 59 (9) 947-51
- Wang et al: ‘Levetiracetam is associated with a decrease in subclinical epileptiform discharges and improved cognitive functions in pediatric patients with autism spectrum disorder’, Neuropsychiatr Dis Treat 13:2321-26, 2017
- Suzuki et al, 2013: ‘Microglial activation in young adults with ASD’, JAMA Psychiatry 70 (1) 49-58


